Lucy Sim, Assistant Director of Medical Physics at Radiation Oncology Princess Alexandra - Raymond Terrace (ROPART), is one of the people behind life-saving cancer treatments in Brisbane. Lucy, who works at one of the two campuses of radiation oncology services in the area, has an extensive role in education and research within the department.
“My role is primarily focused on education and research. I look after post-graduate student projects and supervise registrars. The registrar program is a three-year program where they get hands-on experience, and by the end, they can operate independently as medical physicists,” said Lucy.
One of the key responsibilities as a medical physicist is ensuring the safe, precise, and effective delivery of radiation therapy.
“We look after the bunker in terms of shielding, ensuring the surrounding area is safe for both the staff and the public. We also provide advice on radiation safety regarding patients coming in from scans such as PET imaging.”
Medical physicists also play a vital role in ensuring high-quality radiation doses. A key part of this is the commissioning and quality assurance of radiation therapy equipment. Currently, Lucy and her team are working on the commissioning of a new TrueBeam linear accelerator, a complex process that can take several weeks to complete but is crucial for delivering high-quality cancer care.
“We do a huge range of measurements to calibrate the machine. This is to ensure that the beam we use is as precise as possible to treat the tumour,” she said.
Lucy also works in a multidisciplinary team of radiation oncologists, radiation therapists, nurses, and engineers to embed new technology into our treatment workflow. One example is a new surface guidance system to improve patient positioning during radiation therapy.
“Patients need to be positioned the same way each day to ensure radiation targets only the tumour and spares healthy tissue,”
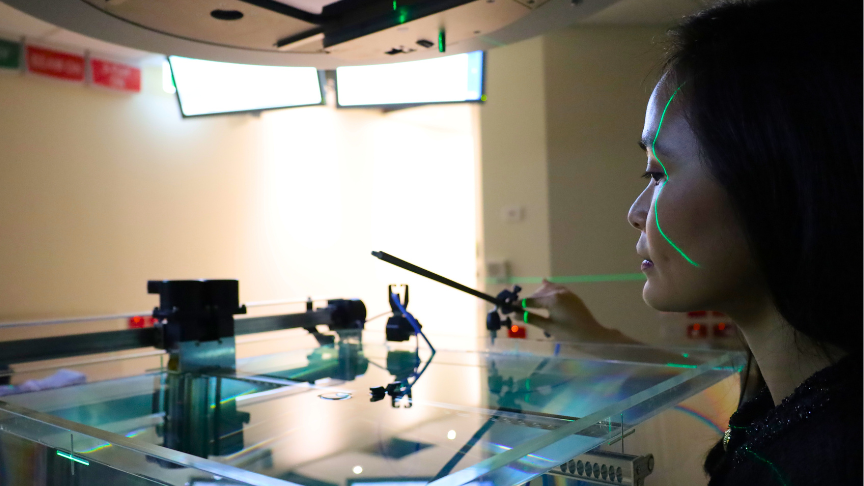
Traditionally, vacuum bags and CT scans were used to confirm positioning. Now, with the new optical surface scanner, a light pattern is projected onto the patient's skin, allowing the team to verify positioning without using any radiation.
“This system is faster, safer, and more comfortable, especially for patients receiving daily treatments.
“It also offers multicultural inclusivity by accurately tracking all skin tones, ensuring equitable care for diverse patient populations.”
The new technology also offers the potential to eliminate the need for permanent tattoos, which are often used to mark patient positioning.
“For some patients, permanent tattoos can be distressing, so being able to offer tattoo-free treatments respects cultural sensitivities and significantly improves the emotional experience for patients.”
Beyond her clinical work, Lucy is committed to fostering the next generation of medical physicists. She actively contributes to building the pipeline of talent through a wide range of education and mentorship initiatives.
“What I love about medical physics is that it combines different skills. Some people gravitate toward coding and scripting, others thrive on writing, analytical skills, or collaboration. And you don’t need to be in one specific box—you can really create your niche within the field,” she explains.
“I genuinely care about what I do. I love knowing that the work I’m doing is directly impacting patients and improving their quality of life. Even with the long hours, I know it’s all worth it.”